An analysis of sputum secreted by patients when coughing is often used. In addition, valuable diagnostic information can be obtained by examining washings obtained during bronchoalveolar lavage, as well as pleural effusion (fluid in the cavity surrounding the lungs). Read about what kind of research this is, who needs it, how it is conducted and how it is interpreted.
Sputum is the secretion of glands located in the walls of the trachea and bronchi. Normally, there is little of it; it is excreted using the cilia of the ciliated epithelium unnoticed by humans and is swallowed. With pathological processes in the respiratory system, the amount of sputum increases, its properties change, it begins to separate when coughing or expectoration, mixing with secretions from the nasopharynx and saliva.
To study this secret, use general analysis sputum. Bacteriological research is also carried out, including determining the sensitivity of isolated microorganisms to antibiotics.
For what diseases is a general sputum analysis performed?
- inflammatory processes (acute bronchitis);
- specific processes (tuberculosis, sarcoidosis);
- chronic respiratory diseases (bronchiectasis, chronic obstructive pulmonary disease);
- bronchial and lung cancer;
- silicosis, Goodpasture's syndrome, echinococcosis, actinomycosis and some other conditions.
The study is not performed for pulmonary hemorrhage.
How to take a sputum test:
A sputum test is taken after waking up
- sputum is collected in the morning after getting out of bed, before this you should not drink, eat, smoke, take medications, or brush your teeth;
- before collecting sputum, the patient should rinse his mouth well, preferably with boiled water;
- you need to strive to ensure that nasal and pharyngeal mucus does not get into the material;
- after several successive deep breaths, expectorate the sputum and spit it out into a sterile jar, which is closed with a plastic lid or thick paper secured with an elastic band;
- the resulting material is quickly delivered to the laboratory.
Interpretation of the results obtained:
- Normally, sputum is mucous. An admixture of pus occurs with the appropriate nature of the inflammatory process in chronic bronchitis, severe pneumonia, bronchiectasis, and lung tumors. Purulent sputum appears when a lung abscess has opened into the lumen of the bronchus, a suppurating echinococcal cyst, or an exacerbation of bronchiectasis.
- Blood is recorded in case of bleeding caused by tuberculosis, disintegrating tumor, exacerbation of bronchiectasis, pulmonary infarction. Hemoptysis occurs with syphilitic lesions, organ contusion, lobar pneumonia, silicosis, heart failure with left ventricular failure.
- Normally, sputum is colorless or whitish in color. The greenish tint of sputum indicates its purulent nature. If the sputum has a rusty appearance, this means that it contains decayed red blood cells, which are released in cases of lobar pneumonia, tuberculosis, pulmonary infarction, and also in severe heart failure.
- A putrid odor is noted in sputum analysis in cases of abscess, bronchiectasis, gangrene, and disintegrating lung cancer.
- If the sputum has an acidic environment (pH less than 7), this indicates too long a time has passed between taking the test and studying it, when the sputum has time to decompose. A large amount of protein is characteristic of the tuberculosis process.
- During microscopic examination, the most important diagnostic value is the detection of:
- “cells of heart defects” (macrophages that capture blood that sweats into the alveoli during pulmonary infarction and heart defects);
- neutrophils (a sign of purulent sputum);
- eosinophils (for bronchial asthma, pulmonary echinococcosis, tuberculosis, cancer, pulmonary infarction);
- lymphocytes (for whooping cough and tuberculosis);
- a large number of red blood cells is a sign of pulmonary hemorrhage.
- Groups of atypical cells may be found in the sputum - this is a sign malignant tumor bronchi or lung tissue.
- When lung tissue is destroyed, elastic fibers are found in the sputum (tuberculosis, abscess, lung cancer). It is characterized by the detection of Kurshman spirals (casts of small bronchi) and Charcot-Leyden crystals (clusters of eosinophils).
A bacteriological examination of sputum is also carried out: express methods for identifying microorganisms, bacterioscopy (examination of stained smears under a microscope), detection of Mycobacterium tuberculosis, culture on a nutrient medium to determine the sensitivity of pathogens to antibiotics. These tests are performed for infectious diseases of the lungs: pneumonia, bronchitis, bronchiectasis, abscess and gangrene of the lung.

Bacteria in sputum
The most common pathogenic bacteria found in sputum are staphylococci, pneumococci, Klebsiella, and Haemophilus influenzae. So-called intermediate-level pathogens can also be detected - Moraxella, Enterobacteriaceae, and fungi of the genus Candida. They are often opportunistic flora and cause pneumonia or other inflammatory disease of the respiratory tract in people with weakened immune systems. Less common are mycoplasma, Pseudomonas aeruginosa, chlamydia, and legionella. Some of them cause so-called atypical pneumonia.
The number of bacteria in 1 ml of sputum is of clinical importance. It is believed to be 10 6 – 10 7 CFU/ml. CFU is a colony-forming unit, that is, a microorganism capable of reproduction.
If sputum is applied to a nutrient medium using a special technology, then after some time colonies of microorganisms present in the mucus will form on it. They are exposed to various antibacterial substances and it is determined under the influence of which antibiotics the isolated pathogens die. This is how sensitivity to antibiotics is determined. It is clear that such an analysis cannot be carried out quickly. A sputum sensitivity test is done over several days. Without waiting for the result, doctors begin treatment with broad-spectrum antibiotics; after receiving the analysis, therapy can be adjusted.
To determine Mycobacterium tuberculosis, sputum is usually collected for three days in a row. Determination of these pathogens is carried out either by microscopy of a stained smear, or by inoculation on nutrient media. The result in this case can be obtained only after 14–90 days, but it will be very informative. It will be possible not only to confirm bacterial excretion, but also to obtain data on the sensitivity of the pathogen to antibacterial agents.
An additional method for diagnosing tuberculosis is infection of laboratory animals with material obtained from sputum.
The detection of Mycobacterium tuberculosis in sputum indicates its “open” forms, in which the patient is infectious to others.
Bronchoalveolar fluid analysis
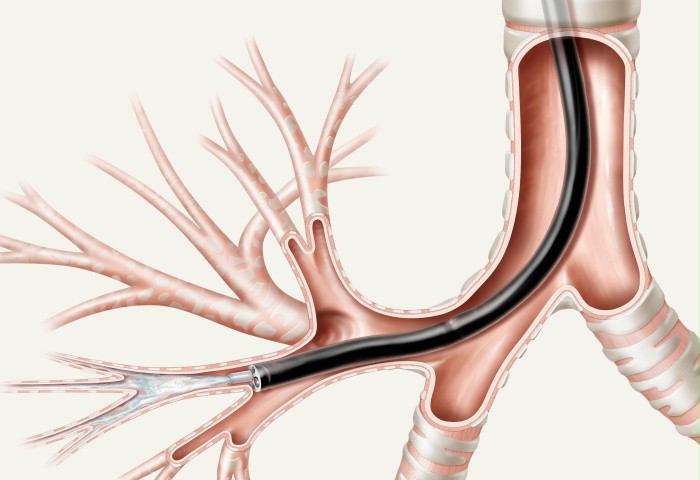
Bronchial and bronchoalveolar lavages are examined. To obtain them, you need a fiber bronchoscope - an endoscopic device with a thin tube inserted into the bronchial tree. An even thinner catheter is passed through the bronchoscope channel. A sterile saline solution is then injected through it and completely aspirated back, thereby obtaining washouts from the surface of the wall of the segmental bronchi or smaller bronchi and alveoli. This depends on the depth of insertion of the bronchoscope.
The resulting liquid is analyzed under a microscope. It counts the number of epithelial cells, macrophages, neutrophils, lymphocytes, eosinophils and others.
Normal cell content in bronchoalveolar fluid analysis:
- macrophages – 87%;
- lymphocytes – 12%;
- neutrophils – 0.5%;
- eosinophils – 0.5% (Chernichev L.A., 1996).
The study is carried out only in specialized centers as an addition to other methods for recognizing nonspecific pulmonary diseases. It helps in the differential diagnosis of the following diseases:
- bronchial asthma (increased eosinophil content up to 9%);
- eosinophilic pneumonia (increased eosinophil content up to 23%);
- sarcoidosis (increased lymphocyte content up to 40%);
- (increase in neutrophil content up to 7%);
- chronic bronchitis (increased neutrophil content to 69%).
In the analysis of bronchoalveolar lavages, as well as in sputum, the presence of microorganisms and their sensitivity to antibiotics are determined. The clinically significant number of microbes is at least 10 4 – 10 5 CFU/ml. If a smaller number of microorganisms are detected, it is considered that they are “not involved” in the occurrence of the disease in the patient being examined.
Pleural effusion analysis
- fluid in the pleural cavity that accumulates in pathological quantities. The pleural cavity consists of two layers of pleura, the inner one is adjacent to the lungs, and the outer one is adjacent to the chest wall. Between them there is normally up to 20 ml of fluid, which ensures the sliding of the pleura relative to each other and the free movement of the lungs during breathing. Under various pathological conditions, the amount of pleural fluid increases, and then it is called pleural effusion.
Pleural effusion can be a transudate or an exudate. Transudate appears when high blood pressure in the veins or low protein content in the blood, the lungs are not affected, there is no inflammation.
When is the study carried out?
Reasons for the appearance of transudate:
- chronic heart failure of III – IV functional class, with a significant decrease in the contractility of the heart;
- a pronounced decrease in the amount of protein in the blood, in particular, when its synthesis is impaired (liver cirrhosis) or when there is increased excretion in the urine (nephrotic syndrome in kidney disease);
- concomitant ascites (accumulation of fluid in the abdominal cavity) with Meig's syndrome, hypothyroidism.
Exudate appears when the permeability of the pleural capillaries increases and indicates damage to the lungs and/or pleura:
- metastases into the pleura of a tumor of the lung, breast or other organs, lymphogranulomatosis, tumor of the pleura itself (mesothelioma), non-Hodgkin's lymphoma;
- pneumonia and tuberculosis;
- pulmonary infarction;
- diffuse connective tissue diseases;
- lung injury, hemothorax;
- Dressler's syndrome, which develops in the first month after myocardial infarction;
- other conditions.
To differentiate between these diseases, a pleural puncture is performed and pleural fluid is obtained for analysis. If the volume of effusion is large, the fluid is simultaneously evacuated using a special system consisting of a syringe with a shut-off valve and an impenetrable bag for the fluid.
How is a pleural puncture performed?
Special preparation for the study is usually not required. Before puncture, it is advisable to empty the bladder, especially if fluid evacuation is expected (this takes an average of 30 minutes).

Pleural puncture
The patient sits on a chair facing the back, tilts his head forward, and places his hands on the back of the chair. The site of the intended puncture is treated with alcohol and an injection of novocaine is given. Then, in the area of the 6th - 7th intercostal space along the mid or posterior axillary line, a needle is inserted for pleural puncture and fluid is obtained for analysis; if necessary, the effusion is gradually removed.
After removing the needle, the puncture site is treated with alcohol, tincture of iodine, covered with a sterile napkin and sealed with an adhesive plaster. In some cases, tight bandaging of the chest is additionally performed. The patient must remain in bed for 24 hours.
Interpretation of results
The resulting pleural fluid is assessed according to several criteria:
- protein content: when its level is more than 3 g% or the ratio with serum protein is more than 0.5, we speak of exudate;
- leukocyte content less than 1 * 10 9 / l is a sign of transudate, more than 1 * 10 9 / l is exudate, if lymphocytes predominate, a tuberculous or tumor process can be suspected; when the number of leukocytes is more than 100*10 9 /l they speak of pleural empyema;
- eosinophils are often observed in tuberculosis, drug-induced pleurisy, Dressler's syndrome;
- the number of red blood cells more than 100 * 10 9 / l is a sign of blood penetration into the pleural cavity due to a tumor, injury or pulmonary infarction;
- the amount of glucose less than 3.3 mmol/l is observed with pleural empyema and pleurisy accompanying rheumatoid arthritis;
- A pH less than 7.2 (acidic reaction) is recorded with pleural empyema;
- an increase in the amount of amylase of more than 500 U/ml occurs with acute pancreatitis or perforation of the esophagus;
- a fat content of more than 5 g/l indicates chylothorax.
Also, atypical cells are determined in the pleural fluid - a sign of a pleural tumor or metastases to it. In addition, bacterioscopy and bacteriological examination are carried out to identify microorganisms that cause the disease, including mycobacterium tuberculosis. The latter, even with the known tuberculous nature of the effusion, are not always found.
The video describes the laboratory diagnosis of tuberculosis:
Clinical examination of sputum includes the study of physical (macroscopic), chemical properties, as well as microscopic, bacterioscopic and bacteriological studies.
When conducting a general clinical analysis of sputum, it is necessary to remember the rules for collecting material. After thoroughly rinsing the mouth and throat, sputum should be collected into a clean, dry Petri dish in the morning on an empty stomach.
When examining sputum macroscopically, attention is paid to the quantity, color, smell, consistency, layering, its nature, and the presence of various inclusions.
The amount of sputum varies widely depending on the nature of the disease. Thus, a meager amount of pathological secretion is released during tracheitis, acute bronchitis, bronchial asthma and bronchopneumonia. Abundant - in case of cavity processes in the lungs (bronchiectasis, abscess, gangrene).
Layering. Two-layer sputum (pus and plasma) is characteristic of a lung abscess, three-layer (pus, plasma and lumps of mucus on the surface) - for bronchiectasis, cavernous pulmonary tuberculosis.
The nature of sputum is determined by the presence of mucus (mucous sputum), pus (purulent), and blood (bloody). Most often, sputum consists of a mixture of mucus and pus (muco-purulent, purulent-mucous), mucus and blood (muco-bloody). Serous sputum is blood plasma that has sweated into the bronchial cavity and is released mainly during pulmonary edema.
Sputum, consisting of mucus, is released during inflammatory processes (acute bronchitis, bronchopneumonia, bronchial asthma), purulent sputum - with a lung abscess open in the bronchus, bronchiectasis. Bloody sputum is observed with pulmonary hemorrhage (tuberculosis, malignant neoplasms and etc.).
The consistency of sputum can be viscous, thick or thin. When there is a large amount of mucus in the sputum, for example in bronchial asthma, the sputum is viscous. If there are a large number of formed elements, cells (pus), the sputum is thick. With a large amount of sputum and the presence of plasma in it, the consistency becomes liquid.
The color of sputum depends on its consistency and nature. So, mucous sputum is transparent. Mucopurulent - with a yellowish tint, purulent mucous - yellowish-green. Mucous-bloody sputum - with a rusty tint, bloody sputum - red, serous sputum - transparent yellow, foamy.
The smell most often appears when mucus is retained in the bronchi and lung cavities. Freshly secreted sputum is usually odorless. A sharp unpleasant odor of sputum can be with bronchiectasis, lung abscess, foul-smelling - with gangrene of the lung.
Microscopic examination of sputum is carried out in native and fixed stained preparations.
The native drug is examined under a microscope, first at low and then at high magnification. Cellular, fibrous and crystalline elements can be found in the native preparation.
Cellular elements. Flat epithelium is desquamated epithelium of the oral mucosa; it has no diagnostic value, since it is found in almost all subjects.
Columnar epithelium - the epithelium of the mucous membrane of the bronchi and trachea is found in large quantities during an acute attack of bronchial asthma, acute bronchitis.
Macrophages - cells of bone marrow origin are found in various inflammatory processes in the bronchi and lung tissue (pneumonia, bronchitis). The detection of macrophages containing hemosiderin (“heart defect cells”) is of important diagnostic importance; they have golden-yellow inclusions in the cytoplasm. These cells are found in the sputum of patients with congestion in the pulmonary circulation, with pulmonary infarctions, and hemorrhages into the pulmonary tissue.
Leukocytes are round cells with abundant granularity. Occurs in any inflammatory processes in the oral cavity, bronchi, and lungs.
Red blood cells are double-circuited oval-shaped cells of a yellowish color, without granularity. A lot.
Full version methodological manual shown in photographs.
General sputum analysis is a method that helps clarify the diagnosis of diseases respiratory system. Sputum is a pathological discharge that is produced in various diseases of the respiratory system. At the same time, production significant amount the secret says enough serious illnesses in this area.
In this case, a very important indicator is what and whether there are pathological impurities in it. With ordinary acute respiratory viral infections and some other relatively harmless diseases of the respiratory system, a person usually produces light sputum without any impurities.
The main task of sputum is the gradual removal from the respiratory system of microorganisms that caused the development of the disease, their metabolic products, as well as other pathological elements.
Basic indications and preparation
There is enough a large number of pathological conditions, as well as diseases for which sputum examination may be prescribed. The main ones among them are the following:

If necessary, the doctor may prescribe sputum examination for other diseases. The table of pathological conditions in which an excessive amount of this secretion is produced is huge. Moreover, in most cases (except for tuberculosis and some other pathologies) this analysis is optional.
Many of our readers actively use the Monastic Collection of Father George to treat coughs and improve their condition with bronchitis, pneumonia, bronchial asthma, and tuberculosis. It contains 16 medicinal plants that are extremely effective in the treatment of chronic COUGH, bronchitis and cough caused by smoking.
It is better if its direct collection is carried out in a room specially equipped for this purpose. At the same time, for normal control by a specialist, such a room is equipped with a glass partition, behind which the patient is located.
 The doctor observes how the patient coughs up mucus and makes recommendations. If the patient is unable or unwilling to go to a medical facility, he can spit it out into a special container right at home. It is then taken to a specialized laboratory for examination.
The doctor observes how the patient coughs up mucus and makes recommendations. If the patient is unable or unwilling to go to a medical facility, he can spit it out into a special container right at home. It is then taken to a specialized laboratory for examination.
The doctor referring him for this study should tell the patient how to properly collect sputum. It is very important to strictly follow absolutely all of his recommendations, otherwise the result will be unreliable. First of all, the patient should properly prepare for the examination itself.
For more correct collection of sputum for general analysis, you must follow the following rules:
- Sputum should be collected in the morning.
- Before doing this, you need to brush your teeth well and rinse your mouth.
- Then you need to inhale and exhale deeply 3 times.
- You need to spit out the sputum into a special sterile container provided by a specialist, being careful not to let any saliva get into it.
 If the patient does not know how to properly collect sputum for analysis, then there will be a large amount of saliva. Such research will ultimately prove uninformative.
If the patient does not know how to properly collect sputum for analysis, then there will be a large amount of saliva. Such research will ultimately prove uninformative.
To improve sputum discharge, you can drink a cup before the examination. hot water or perform inhalation with soda and salt. By following these simple rules for collecting sputum, the patient will significantly increase the likelihood that he will not have to undergo this examination again.
After collecting sputum for analysis, a comprehensive examination is carried out. It is necessary in order to accurately identify a person’s disease.
 The main stages are the following:
The main stages are the following:
- Clinical analysis.
- Microscopic analysis.
- Bacteriological analysis.
Thanks to this comprehensive approach to this study, it is possible to identify a fairly wide range of different pathologies.
A clinical study of sputum analysis involves assessing the following parameters:
- total amount;
- color;
- smell;
- the presence of pathological impurities.
Clinical analysis of sputum allows you to obtain certain data on the nature of the course of the disease in the shortest possible time. A specialist can immediately determine how large an amount of biological material was delivered, what color and smell it has, and whether there are any impurities in it.
 Microscopic analysis involves studying sputum under multiple magnification. This makes it possible to identify eosinophils in sputum, leukocytes, Charcot crystals and other elements. The presence of such pathological particles in a given biological material may indicate the development of quite serious diseases.
Microscopic analysis involves studying sputum under multiple magnification. This makes it possible to identify eosinophils in sputum, leukocytes, Charcot crystals and other elements. The presence of such pathological particles in a given biological material may indicate the development of quite serious diseases.
As for bacteriological analysis, it is necessary to determine the presence of various pathogenic microorganisms in a sputum sample, as well as to determine their specific variety. This method studies are used when large numbers of leukocytes are detected in sputum.
In order to carry out the research at this stage, bacterial inoculation on nutrient media is used. After some time, a colony of microorganisms grows. In this form, it is much easier to identify a specific pathogen.
In addition, bacterial culture of sputum makes it possible to clarify which antimicrobial agents a particular pathogen is sensitive to. This helps prescribe a rational course of treatment. Currently, sputum culture is most often performed when pulmonary tuberculosis is suspected.
Decoding the received data
If the patient was correctly informed about how to take this type of analysis, then the specialist will receive a sufficient amount of useful information.
 The absolute norm for such a study involves determining the following parameters:
The absolute norm for such a study involves determining the following parameters:
- Absence of pus and other pathological impurities, as well as particles.
- A transparent, homogeneous substance that is mucus.
- No foul smell.
If the examination of sputum makes it possible to determine the presence of a sufficiently large number of eosinophils, whose number exceeds 50% of all leukocytes present in the sample, then most often we are talking about diseases such as:
- bronchial asthma;
- allergic infiltrate;
- helminthic infestation of the lungs.
In cases where the collected material contains more than 25 neutrophils, then most likely the patient has developed infection lungs or bronchi.
 Quite often this picture is observed when:
Quite often this picture is observed when:
- pneumonia;
- acute and chronic bronchitis;
- tuberculosis.
In this case, subsequent sputum culture is necessarily carried out to determine the specific microflora and its sensitivity to certain antibacterial drugs. In this case, sputum culture will not provide the necessary information urgently. It will take some time for colonies of pathogenic microorganisms to form.
If more than 25 squamous epithelial cells are detected in the test material, we can say that the sputum collection was carried out with violations. In addition, such an analysis will most likely contain a fairly large amount of saliva.
If, when deciphering a sputum analysis, accumulations of elastic fibers are detected, this may indicate the beginning of the process of decay of lung tissue. This is observed with widespread tuberculosis or abscess pneumonia.
 Kurshman spirals are formed in various types of bronchospastic syndrome. Most often, these elements are determined in bronchial asthma. Kurshman spirals are casts of the smallest bronchi. Such particles are often detected in fairly thick sputum. Kurshman spirals are one of the important diagnostic signs of the presence of bronchial asthma in a patient.
Kurshman spirals are formed in various types of bronchospastic syndrome. Most often, these elements are determined in bronchial asthma. Kurshman spirals are casts of the smallest bronchi. Such particles are often detected in fairly thick sputum. Kurshman spirals are one of the important diagnostic signs of the presence of bronchial asthma in a patient.
Charcot-Leyden crystals are also evidence that the patient has bronchial asthma. These particles are rather elongated thin formations, similar to crystals. They consist of enzymes that are secreted by eosinophils.
Charcot-Leyden crystals have a shiny, smooth, almost colorless surface. Moreover, even if the analysis failed to show the presence of such particles, this does not mean at all that the person does not have bronchial asthma. Leiden cells may not be present in fresh sputum.
For analysis in this case, it is important that 24-30 hours pass. After this time, these particles should already be formed from decaying eosinophils. In this case, it is better to collect sputum during the interictal period.
 Almost anyone can submit sputum for analysis. Moreover, if you know how to properly take a sputum test, it will turn out to be the most informative for many diseases. There are no contraindications to this study.
Almost anyone can submit sputum for analysis. Moreover, if you know how to properly take a sputum test, it will turn out to be the most informative for many diseases. There are no contraindications to this study.
The only limitation is the person's physical disability. It's about about children and patients with severe weakness bordering on immobility. In addition, patients who have suffered a stroke and have swallowing disorders often cannot take it.
Sputum analysis- studying physical signs, qualitative, quantitative composition, as well as bacteriological and cytological properties of sputum.
U healthy person A small amount of protective mucus is produced in the respiratory tract every day. During illness, the amount and composition of discharge changes significantly. In addition to mucus, pathogenic microbes, blood cells (erythrocytes, leukocytes) and other specific components accumulate in it. This discharge is called sputum.
Sputum analysis provides the doctor with information about the stage, nature and localization of the process in the lungs, and allows for differential diagnosis among a variety of respiratory diseases. In some cases, a sputum test is ordered to look for cancer cells (sputum cytology) or tuberculosis bacteria (sputum TB test). With the help of bacteriological examination of sputum, it is possible to detect the causative agent of the disease and accurately select an antibiotic, the treatment of which will be most effective in this case.
In what cases is sputum analysis prescribed?
- prolonged cough with sputum;
- diagnosis of acute (bronchitis, pneumonia) and chronic (COPD, bronchial asthma) lung diseases;
- monitoring the effectiveness of treatment of respiratory diseases;
- suspected pulmonary tuberculosis;
- suspected lung cancer;
- suspicion of helminthic infestation of the lungs.
How to properly collect sputum
Sputum is collected in a medical facility, or independently - at home. After collection, it must be delivered to the laboratory at as soon as possible(1-2 hours). You must first purchase a sterile, sealed container.
Before collecting sputum, you need to brush your teeth and rinse your mouth thoroughly. Cough and collect the secretions in a container. It is necessary to minimize the entry of saliva into the material.
To make phlegm come out easier:
- on the eve of the analysis, it is recommended to drink plenty of warm drinks;
- the analysis is given in the morning;
- you need to take three deep breathing movements and then cough;
- in case of unsuccessful attempts, inhalation over water vapor with the addition of table salt and baking soda within 5-7 minutes.
Normal values for sputum analysis
Normally, sputum is not produced at all.
Interpretation of sputum test results
The physical properties of sputum allow us to judge the cause and stage of the disease.
- Mucous, viscous, transparent sputum is more characteristic of a viral infection of the respiratory tract. Can be observed with ARVI, acute bronchitis.
- Cloudy sputum, white, yellow-green, contains pus. Characteristic of many inflammatory lung diseases (pneumonia, lung abscess), exacerbation of chronic obstructive bronchitis, bronchial asthma. However, sputum can become purulent as a result of diseases of the ENT organs (rhinitis, sinusitis).
- Amber-colored sputum may indicate an allergic nature of the disease.
- Sputum mixed with blood is an alarming sign; it can be observed with tuberculosis, lung cancer, systemic connective tissue diseases, etc. However, streaks of blood may appear in the sputum during severe hacking cough (tracheitis, whooping cough), when the mucous membrane of the respiratory tract is injured during coughing movements.
When examining sputum under a microscope, the cellular composition can be determined.
- The detection of neutrophilic leukocytes in the sputum - more than 25 cells in the field of view - indicates infectious inflammation. If a large number of eosinophils are detected (more than 50-90%), an allergic nature of the disease or helminthic infestation is assumed.
- Detection of Charcot-Leyden crystals and Courshman spirals in sputum often indicates the development of bronchial asthma.
- A dangerous sign is the presence of elastic fibers in the sputum, which occurs when lung tissue is destroyed (for example, with abscess pneumonia, cancer, tuberculosis).
- Detection of atypical cells during cytology is a sign of a probable malignant process in the lungs.
In bacteriological examination of sputum, the microbial composition is studied. Normally, saprophytic flora is sown, which does not cause harm to humans, such as staphylococcus, streptococcus and other bacteria.
The detection of pathogenic species in quantities greater than 106 in 1 ml indicates the possible role of this microbe in the development of the disease. In this case, the pathogen is inoculated on media with various antibiotics and the most effective one is determined.
Sputum accumulates in the respiratory tract and is a pathological discharge from the mucous membrane of these canals. During coughing, the accumulations are expelled. Due to various diseases, sputum may have a different microbiological composition. Analysis of this composition will make it possible to predict or identify with an accuracy of one hundred percent the causes of pathological abnormalities in the respiratory tract or lung tissues. How to take a sputum test - read on.
Who needs a sputum test?
This test may be prescribed to patients who have had respiratory discharge for a long period of time. Another indication is if a chest x-ray shows shadows of unknown origin.
Preparation for analysis, sputum collection
Sputum collection is carried out in the morning, before the first meal. It is necessary to carefully prepare the body for the test: rinsing the oropharynx, spitting saliva as much as possible. Substances required for analysis must be coughed out, and there should be no products of the salivary glands or secretions from the nasal cavity in the samples.
The patient takes in more air through the mouth and begins to cough for a long time. The excreted secretions are spat into a previously prepared sterile container, then the container is sealed and the sample is delivered to the laboratory.
If, when coughing, the amount of sputum released is insignificant, then irritating inhalations (potassium or potassium iodide) can be additionally used to increase sputum production. For greater efficiency in diagnosing and prescribing treatment, such an analysis should be taken several times (throughout the entire disease).
Sputum examination, interpretation of results
For a thorough examination of sputum, it is very important to know its quantity; in some cases, the size of the secreted substances can reach several liters per day. This is observed with lung abscesses, bronchiectasis, and the presence of a tuberculous cavity.
Depending on the type of disease, the composition of the discharge will be different. Mucous sputum is released in acute bronchitis, bronchial asthma, mucopurulent or purulent discharge is observed in bronchitis, inflammation and abscesses of the lungs, bronchiectasis. In severe forms of the disease, blood impurities may be released along with sputum: from a few droplets in the form of blood streaks to clots or the main coughing up of blood mixed with mucus and tissue detritus. Bloody discharge is a clear sign of tuberculosis, lung cancer or infarction, bronchiectasis, lobar pneumonia and some other serious diseases. With pulmonary edema, the sputum also contains other liquid components (serous sputum). If tissue decay occurs in the respiratory organs, then over time the sputum will acquire an unpleasant, putrid odor.
The resulting sample is further assessed for delamination. The liquid is allowed to settle, as a result of which three layers can form in case of putrefactive processes or two layers in case of purulent ones. Next, a test is carried out for the chemical reaction of the substances and the protein level is determined.
In some cases, additional studies of sputum are also carried out: a smear of secretions is applied to a glass slide, then the substance is stained in accordance with the analysis procedure and placed under a microscope. Here it is already possible to identify smaller components: bacteria, fibrous and cellular elements. This study of the composition of sputum reveals: microscopic cells of the bronchial epithelium, macrophages of the alveoli with various inclusions, red blood cells, types of leukocytes, eosinophils, cancer cells, fragments of fibers, and so on. For different diseases, the microscopic composition of sputum varies. In rare cases, Charcot-Leyden crystals, Courshmann spirals and a number of other elements are found in the discharge.
To prescribe antibiotics to a patient, sputum is cultured: the secretions are placed in a nutrient medium for the growth of colonies of microorganisms, which are then tested for sensitivity to the drugs.

