Depending on the location of the affected area, pneumonia can be unilateral or bilateral: with unilateral inflammation, it affects only one lung, with bilateral inflammation, both. In right-sided pneumonia, the right lung is affected.
Right human lung anatomically somewhat different from the left. Firstly, it is shorter and somewhat larger in volume. Secondly, the right lung is divided by interlobar fissures into three lobes - upper, middle and lower, while in the left there is only one interlobar fissure, and, accordingly, only two lobes - upper and lower.
If inflammation affects the entire lower lobe of the right lung (the pleura, the lining of the lungs, can also be involved in the process), we can talk about right lower lobe pneumonia.
If the area of inflammation does not extend to the entire lobe, it may be limited to one or more of its segments or one lobe of the lung - in these cases, segmental or lobular pneumonia is diagnosed.
Features of lower lobe right-sided pneumonia
Inflammation of the right lung is more common due to anatomical structure bronchi - the right bronchus is shorter and wider than the left, so the infection spreads faster through it. Following the damage to the bronchi, focal damage to the lung tissue develops, and it is in the right lung that several foci of inflammation can simultaneously be located at different stages of development. This explains the typical course of right-sided pneumonia - the disease proceeds in waves; after a period of temporary improvement, the patient’s condition may deteriorate again.
Inflammation of the lower lobe of the lung may be accompanied by symptoms similar to those of an “acute abdomen” - inflammation of the peritoneum, which to some extent complicates the diagnosis of the disease.
Symptoms of right lower lobe pneumonia
Lobar pneumonia, as a rule, begins acutely - with high temperature, severe chills, sweating. When coughing, viscous sputum is produced, sometimes having a “rusty” orange tint. Any physical exercise cause severe shortness of breath in patients.
Chest pain can occur both when coughing and when trying to take a deep breath. Most often, pain is localized in the area of the affected area of the lung and means that inflammation has affected the pleura.
Right lower lobe pneumonia, like some other types of pneumonia, in some cases occurs in an erased form - the symptoms are mild or absent. Such pneumonia is extremely dangerous, especially if we're talking about about a child’s illness – the risk of complications increases several times due to the inability to diagnose the disease in time. Usually, pneumonia is treated in a hospital setting, however, if the patient’s condition allows and there are no complications (pleurisy, heart or pulmonary failure, bronchial obstruction), pneumonia can be cured at home under the supervision of a local doctor.
Considering the increase in the incidence of colds in children over the past few years (this is associated with a total weakening of the immune system due to poor nutrition, illiterate antibiotic therapy and the use of immunomodulators, the use of which is under strict control throughout the civilized world), doctors often have to diagnose right-sided pneumonia in a child.
Pneumonia is, literally translated from Greek, inflammation of the lungs (parenchyma).
There are several options for classifying this disease. The first classification takes into account the mechanism of occurrence of the disease. According to her, pneumonia can be:
Regarding the course of the disease, pneumonia is divided into four categories, according to which the patient’s management tactics are determined (applies only to community-acquired pneumonia):
- The first clinical group is pneumonia with a relatively mild course (always one-sided), with low-grade fever, and no respiratory failure in people who get sick no more than once a year. It is treated on an outpatient basis (that is, at home).
- The second clinical group is pneumonia of moderate severity, with fever up to febrile levels, and no manifestations of respiratory failure. You can also treat at home.
- The third clinical group is severe pneumonia, with febrile fever; children often experience febrile convulsions (which is especially dangerous with concomitant neurological symptoms). Respiratory failure of the first degree (determined by the frequency of respiratory movements). Hospitalization to the infectious somatic department is required as an emergency.
- The fourth group is the most severe pneumonia, with severe fever, loss of consciousness, febrile convulsions, and stage 2 respiratory failure. Hospitalization to the intensive care unit is required.
Pneumonia (bronchopneumonia) is divided according to the localization of the source of the process - that is, it can be bilateral (lobar) - polysegmental, segmental right-sided (the article is actually about it) or segmental left-sided. Further, bronchopneumonia is already divided with clarification by segment - upper lobe, middle lobe or lower lobe (this is only for the left lung, right-sided pneumonia (bronchopneumonia) can only be upper or lower lobe due to the anatomical features of the bronchial tree).
That is, it becomes clear from all of the above that to understand the pathological process you need to know all its features, which is reflected in the classification of this disease. Taking into account the topic of the article, let's derive the correct diagnosis (example):
Acute out-of-hospital right-sided polysegmental pneumonia, clinical group 3, respiratory failure 1.
Regarding the division according to the degree of intensity of the process, chronic pneumonia is distinguished, but this is only in theory, because in practice no one has ever seen this disease. At least in children this is for sure.
The process of inflammation in the lungs.
By the way, during the sensational epidemics of swine and bird flu, people mostly died from polysegmental pneumonia, which was a bacterial complication of influenza infection.
This disease (in most cases) is not primary, but represents the descent of a viral infection from the upper to the lower respiratory tract.
That is, at first the child seems to fall ill with an acute respiratory viral infection (ARVI, a cold, in popular parlance), few people pay attention to this, the patient does not receive adequate therapy, then the infectious-inflammatory process descends into the trachea, bronchi (occurs bronchitis, which is accompanied by a strong cough, usually dry). And from there, through the alveolar capillary network, the infection spreads into the lung parenchyma and a focus of inflammation occurs, called pneumonia.
Or by aspiration. When swallowing vomit, it enters the respiratory tract with all the ensuing consequences.
Diagnostic standards
The figure shows the focus of inflammation in the lungs.
It all starts with collecting complaints from the child or from the parents. With pneumonia (no matter segmental left-sided or segmental right-sided, bronchopneumonia), a sick child will complain of increased body temperature, cough with sputum, sometimes pain in the chest, difficulty breathing (the last two are unfavorable prognostic signs). A history (medical history) will most likely include hypothermia or contact with another sick child. As a rule, the patient will experience catarrhal and hyperthermic syndrome with bronchopneumonia for several days. The objective picture of the disease will mainly consist of listening to hard breathing and moist fine rales over the entire surface of the lungs. On percussion, children will notice a dullness of sound over the affected area (correspondingly, with segmental right-sided pneumonia - on the right, segmental left-sided pneumonia - on the left). In this case, children may have a weakening of vocal tremor in the same area.
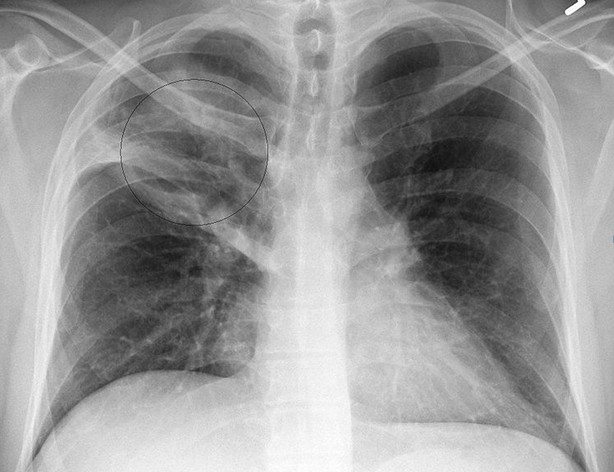
Pneumonia can be confirmed by a chest X-ray (you should not refuse to conduct this study in a child, citing radiation - in any case, it is justified here).
Basic principles of therapy
 This disease is serious and in any case, consultation with the attending physician is necessary. In the cases mentioned above, focal pneumonia can be treated at home, but it is still better to be in hospital with the child, under the round-the-clock supervision of medical personnel.
This disease is serious and in any case, consultation with the attending physician is necessary. In the cases mentioned above, focal pneumonia can be treated at home, but it is still better to be in hospital with the child, under the round-the-clock supervision of medical personnel.
The basis of treatment in children in this case is the use of antibacterial drugs.
Treatment of bronchopneumonia (focal) should begin with protected penicillins - for a child this is amoxiclav 500 (in suspension), the dosage is calculated individually depending on age and body weight, a dosage scale is attached to the instructions. If over the past six months this patient has been prescribed Augmentin, Amoxiclav or Ospamox, then it is better to prescribe treatment with Zinnat or Cefix - stronger antibiotics, although two to three times more expensive. In this case, there is no need to think about it. IN Lately Cases of microorganisms becoming resistant to these antibiotics have become more frequent (we can speak of ineffective treatment if persistent hyperthermia is observed within 72 hours). In this case, it is necessary to prescribe an antibiotic from the macrolide group (Ormax, Klacid, Sumamed) for the treatment of bronchopneumonia (focal) or switch to injection forms. These antibiotics can also be used as initial therapy for the treatment of pneumonia, especially good for children under one year of age. By the way, with this approach, atypical flora that is insensitive to penicillins and cephalosporins will be eliminated.
If there is pneumonia of the third or fourth clinical group (even if it is right- or left-sided bronchopneumonia, and not lobar), hospitalization and the use of antibacterial therapy by injection (intravenous bolus or in a dropper, this is how vancomycin is administered) are urgently required. No matter what the Americans write about the equivalence of oral and parenteral forms in children under one year of age, injections are much more effective in treatment. In most cases, children are given zinnat or ceftriaxone in an age-specific dosage.
The temperature should be reduced only when it reaches 38 degrees. Use nurofen (syrup) in the treatment of children - age-specific dosage, analdim in suppositories (not allowed until one year), in extreme cases, a lytic mixture, analgin, diphenhydramine and papaverine in equal parts (injection). 
You need to be careful with detoxification therapy (especially in children) - you can administer saline solution, glucose or rheosorbilact. Especially with concomitant acetone syndrome. In parallel with antibiotics, children must be given a probiotic (Linex, yogurt or lactovit) 1 capsule three times a day, children under one year old should be given enterozermine.
You need antitussive drugs - ambroxol or erespal, in syrup (for children under one year old) or tablets (for older children).
conclusions
Pneumonia - dangerous disease in children, the success of treatment depends directly on timely initiation of infusion therapy. Fundamental in the treatment of pneumonia in children is the etiology and severity of clinical symptoms, and not the localization of the pathological process - it does not matter whether right-sided upper lobe or left-sided lower lobe pneumonia is treated in the same way in a child.
A disease such as pneumonia is a severe pathology that can cause serious complications not only in the bronchopulmonary system (reactive pleurisy, pulmonary edema), but also affect other vital organs (purulent endo- and pericarditis, intoxication psychosis, meningoencephalitis, brain abscess , heart failure). IN old times pneumonia and death were inseparable concepts. Even after the discovery of penicillin, it is not always possible to cope with severe forms of this disease. Damage to lung tissue and subsequent inflammation can be focal, covering the entire pulmonary area, or lobar, in which inflammation is localized in one or more lobes of this respiratory organ. If pathological changes cover any segment of the lower part of the lung, then this form of the disease is called lower lobe pneumonia. The symptoms and treatment of this disease differ little from other types of lobar pneumonia, but still some specific features available.
Right-sided and left-sided pneumonia
It is well known that the causative agents of inflammation of the lung tissue can be both viruses and bacteria. Inflammation of the lower lobe of the lung is most often caused by strains of pneumococcal infection that are able to penetrate the respiratory organ through the bronchogenic or hematogenous route. In pulmonological practice, a distinction is made between right-sided and left-sided lower lobe pneumonia. In the first case, the pathological process is localized in the lower right region of the lung, in the second - in the lower left part. Due to the peculiarities of the anatomical structure (the right bronchus is larger and more susceptible to infection), right-sided lesions of the lower pulmonary lobe are more often diagnosed. In turn, left-sided pneumonia predominantly develops against a background of weakened immunity, after suffering from respiratory viral diseases, influenza, hypothermia, and stress. In both cases, the radiograph shows foci of infiltration of the lower pulmonary parenchyma.
Symptoms
Typically, signs of lower lobe pneumonia begin to appear suddenly and acutely, although sometimes mild symptoms are observed with left-sided pneumonia. As a rule, a sick person’s temperature rises to 38–40°C, which is accompanied by headache, shortness of breath, increased sweating, and chills. When taking a deep breath, the patient feels pain in the chest (right or left half). At first, the cough is unproductive, dry, but literally after a couple of days, viscous purulent-mucous sputum with blood streaks begins to leave. The inflammatory process is also characterized common features intoxication: weakness, loss of appetite, nausea, vomiting, muscle pain, decreased blood pressure, cyanosis (blue discoloration of nails and lips). The presence of high fever, rapid breathing, listening to a dull percussion sound and moist rales in the lung area require placement of the sick person in the inpatient pulmonology department of the hospital.
Treatment
When lower lobe pneumonia is diagnosed, the patient is prescribed strict bed rest and anti-inflammatory therapy is immediately started. If acute respiratory failure develops, the patient is connected to a ventilator. The basis of the treatment process for this disease is antibacterial therapy. To select the most effective antibiotic, it is necessary to do a bacteriological culture of the sputum, but treatment begins immediately, without waiting for its results. For lower lobe pneumonia, combinations of various penicillin antibiotics are used, as well as drugs from the drug group fluoroquinolones, cephalosporins, macrolides, and aminoglycosides. At the same time, symptomatic treatment is carried out with the help of immunostimulating, mucolytic agents, antipyretics (relieving fever and fever), and physiotherapy is prescribed (medicinal magnetophoresis and electrophoresis, pulsed UHF therapy).
The duration of the course of treatment is determined by a pulmonologist depending on the severity of the disease, the speed of recovery of lung function, the positive dynamics of the results of radiographs and laboratory data. Relief from an acute period of inflammation of the lower segment of the lung usually takes 1 to 3 weeks.
To avoid the development of lower lobe pneumonia, symptoms and treatment of this potentially dangerous disease, it is necessary to harden the body from the very beginning. early age, avoid hypothermia, be able to cope with stressful situations, promptly consult a doctor in case of infectious lesions. Be healthy!
The information on our website is informative and educational in nature. However, this information is in no way intended to be a guide to self-medication. Be sure to consult your doctor.
Right-sided lower lobe pneumonia, as a rule, occurs more often than left-sided pneumonia. This picture is observed because the bronchial tree has right side special structure.
The right bronchus is located obliquely from top to bottom, which makes it more accessible to bacteria in the lower part of the lung and the accumulation of large numbers of them in it.
If there are a lot of bacteria, then it is difficult to prevent the onset of inflammation of the pulmonary parenchyma. In this case, antibiotics will not give any results, because the bacteria will multiply faster than die.
It is more difficult to carry out therapy for patients with poor blood supply to the bronchus on the right side.
Also important In the pathological process, bacteria also multiply, causing the pulmonary parenchyma to become inflamed.
Right-sided pneumonia should be carefully diagnosed and monitored throughout treatment. If it was caused by pneumococci, then infiltrative foci in the left lung will be visible on x-rays for several days (if the therapy is inadequate or the immune system is weak).
Causes of right-sided pneumonia

The disease occurs due to exposure to various factors and microorganisms on the body. Very often this happens due to the penetration of pathogenic microbes. They cause the following symptoms.
- Symptoms of pneumonia
- How to diagnose right-sided pneumonia?
- Treatment of pneumonia with medications
- Prevention of pneumonia
Right-sided pneumonia is a common lung disease. Pneumonia, also called pneumonia, is characterized by the development of pathogenic microorganisms in a vital human organ. Pneumonia affects the lungs and can be unilateral, that is, localized in one lung, or bilateral. Right-sided pneumonia is most often observed.
Pneumonia is caused by bacteria, viruses and various fungi. In the recent past, the disease was fatal because there were no treatments. But today only a small percentage of people face death. The sooner a doctor diagnoses the disease, the faster recovery will follow.
Causes of right-sided pneumonia
Pneumonia occurs after the body is infected with a virus and is transmitted by airborne droplets. When a person with pneumonia simply sneezes, harmful microorganisms are released and enter the lungs of another person. They then multiply and fill the organ, causing inflammation. It is necessary to use all precautions to avoid infection if someone is sick at home.
 With weakened immune system microorganisms that live on the human mucosa begin to attack the body.
With weakened immune system microorganisms that live on the human mucosa begin to attack the body.
In normal health, there should be no problems, but a weakened immune system cannot overcome them. Thus, the body is affected by bactericidal pneumonia.
The cause of the disease may be fungi that penetrate inside the body and begin to “take over” there. These microorganisms may also be present in a home where there is high dampness.
It is not difficult for them to provoke a disease; it is enough only for the body to be weakened. While for a long time into a room with harmful fungi, the body may well experience negative consequences.
Return to contents
Symptoms of pneumonia
Pneumonia has its own distinctive symptoms that make it possible to make a diagnosis. One of the most important signs of the disease is chest pain when you want to take a deep breath. But there are cases when only one of the symptoms appears, then additional research is carried out.
 Main symptoms of pneumonia:
Main symptoms of pneumonia:
- high body temperature, which indicates an inflammatory process;
- cough, due to which pneumonia can be confused with acute bronchitis;
- runny nose;
- shortness of breath, doctors record tachycardia;
- chest pain when breathing deeply;
- wheezing in the lungs.
Since there are almost no symptoms at the early stage of the disease, there is a certain danger to health. By appearance The patient may notice that he gets tired quickly and has no appetite. Symptoms do not always appear in young children. Parents need to be attentive and sound the alarm in case of any ailments. Children cannot always explain what hurts, so the responsibility to monitor their health lies with the parents.
Return to contents

